The goal of epilepsy treatment is to reduce the frequency and severity of seizures while minimizing side effects and improving overall quality of life. Treatment may involve medications, surgery, or a combination of therapies, depending on the type and severity of the epilepsy.
Medications
Anti-epileptic drugs (AEDs) are the most common treatment for epilepsy. There are many different AEDs available, and the choice of medication depends on the type of epilepsy, the patient’s age and overall health, and other factors.
AEDs work by reducing the abnormal electrical activity in the brain that causes seizures. They can be taken orally in the form of pills or capsules, or injected in the hospital setting. It is important for patients to take their medication as prescribed, at the same time each day, to ensure that the drug levels in the blood remain consistent.
Some of the most commonly used AEDs include:
- Carbamazepine: Used for partial seizures and generalized tonic-clonic seizures.
- Valproic acid: Used for absence seizures and generalized tonic-clonic seizures.
- Lamotrigine: Used for partial seizures and generalized tonic-clonic seizures.
- Levetiracetam: Used for partial seizures, generalized tonic-clonic seizures, and myoclonic seizures.
- Topiramate: Used for partial seizures and generalized tonic-clonic seizures.
- Phenytoin: Used for partial seizures and generalized tonic-clonic seizures.
While AEDs can be very effective at controlling seizures, they can also have side effects such as dizziness, drowsiness, nausea, and coordination problems. Patients should work closely with their doctors to find the right medication and dosage that works best for them.
Surgery
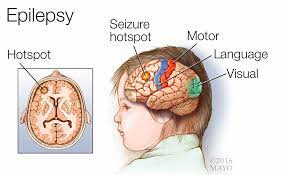
For some people with epilepsy, surgery may be an option. The goal of epilepsy surgery is to remove the part of the brain that is causing seizures while preserving normal brain function. Surgery is typically only considered for patients whose seizures cannot be controlled with medication and whose seizures are localized to a specific area of the brain.
There are several types of epilepsy surgery, including:
- Temporal lobe resection: This is the most common type of epilepsy surgery and involves removing the temporal lobe of the brain, which is often the source of seizures in patients with temporal lobe epilepsy.
- Lesionectomy: This surgery involves removing a specific lesion or abnormality in the brain that is causing seizures.
- Hemispherectomy: This surgery involves removing one half of the brain, typically for patients with severe epilepsy that is affecting one side of the brain.
- Corpus callosotomy: This surgery involves cutting the corpus callosum, the band of nerve fibers that connects the two hemispheres of the brain, to prevent seizures from spreading from one side of the brain to the other.
Surgery can be very effective at reducing or even eliminating seizures in some patients, but it also carries risks such as infection, bleeding, and damage to normal brain tissue. Patients considering surgery should consult with a team of specialists, including a neurologist, neurosurgeon, and neuropsychologist, to determine if surgery is a viable option.
Other Therapies
In addition to medication and surgery, there are several other therapies that can be used to manage epilepsy. These include:
- Vagus nerve stimulation: This therapy involves implanting a device under the skin in the chest that delivers electrical impulses to the vag
- us nerve in the neck, which can help reduce the frequency and severity of seizures.
- Ketogenic diet: This is a high-fat, low-carbohydrate diet that has been shown to be effective at reducing seizures in some patients, particularly children.
- Biofeedback: This therapy uses electronic devices to measure brain waves and provide feedback to the patient, helping them learn to control their brain activity and reduce seizures.
- Cognitive-behavioral therapy: This therapy focuses on identifying and changing negative thought patterns and behaviors that may be contributing to seizures.
- Stress management: Stress can be a trigger for seizures in some patients, so learning stress-management techniques such as meditation, yoga, or deep breathing can be helpful.
- Epilepsy education: Learning more about epilepsy and how to manage it can help patients feel more in control of their condition and reduce stress and anxiety.
- It is important for patients with epilepsy to work closely with their healthcare providers to develop a personalized treatment plan that meets their individual needs. This may involve trying different medications or therapies, adjusting dosages, or exploring surgical options. Regular follow-up visits with a neurologist or epilepsy specialist are important to monitor progress and adjust treatment as needed.
- In addition to medical treatment, there are several lifestyle changes that can help manage epilepsy and improve overall health. These include:
- Getting enough sleep: Lack of sleep can be a trigger for seizures in some patients, so getting adequate rest is important.
- Eating a healthy diet: A well-balanced diet can help improve overall health and reduce the risk of seizures.
- Avoiding alcohol and drugs: Alcohol and drugs can interfere with medication and increase the risk of seizures.
- Wearing a medical alert bracelet: This can alert others to the fact that the wearer has epilepsy and may need help in the event of a seizure.
- Avoiding triggers: Identifying and avoiding triggers such as stress, flashing lights, or certain foods can help reduce the risk of seizures.
- In conclusion, epilepsy is a complex neurological disorder that can be challenging to manage, but there are many treatment options available that can help reduce the frequency and severity of seizures and improve quality of life. These include medications, surgery, and other therapies, as well as lifestyle changes such as getting enough sleep, eating a healthy diet, and avoiding triggers. Patients with epilepsy should work closely with their healthcare providers to develop a personalized treatment plan that meets their individual needs and follow-up regularly to monitor progress and adjust treatment as needed. With the right treatment and support, it is possible to live well with epilepsy.